Women's Health
At BodyThrive Physio we are passionate about helping women of all ages to achieve their optimum physical function and improve their quality of life.

Our Passion

What does a Women’s Health Physiotherapy consult involve?
Listening to your story
Listening to your story and getting to your history, what your issues are and determining your goals and what you would like to achieve is step one. Getting a thorough history taking can assist in giving clues of what might be contributing to your issues, how to help you and to ensure your treatment plan is targeted at achieving your goals.
Assessment
A detailed assessment will be performed to determine what is going on and to guide treatment.
The assessment may involve:
- Pelvic floor assessment.
- Looking at strength, endurance, correct or incorrect contraction of the pelvic floor.
- An internal vaginal examination (if indicated/with consent of the person) can provide comprehensive information on the pelvic floor. It allows us to determine if the pelvic floor is overactive or underactive, gives us a more accurate assessment of pelvic floor strength, and allows us to assess the position of the pelvic organs and determine if any prolapse is present.
- Real Time ultrasound is also used to assess the pelvic floor. This involves using an ultrasound probe on your stomach to locate the bladder and the pelvic floor. This allows you to see your pelvic floor contract and relax on the screen and can be a great feedback tool in training the pelvic floor and reassessing your progress.
- Abdominal muscle separation assessment
- Abdominal strength and function assessment
- Hip strength and function assessment
- Breathing mechanics assessment
Whether you need assistance with strengthening pelvic floor weakness, addressing pelvic organ prolapse, reducing urinary incontinence, having pain-free sexual intercourse, recovering from a vaginal delivery or c-section, or addressing pelvic and low back pain we are here to help.
One in 3 women who have had a baby will experience urinary incontinence, and up to 50% of women who have had a baby will experience some degree of pelvic organ prolapse.
Physiotherapy can play a massive role in the treatment and management of pelvic floor and womens health conditions. Providing education and treatment to help empower women to take charge of their health and improve their quality of life is what Physiotherapy is all about.

Education and Treatment Plan
After the assessment you will be provided with education on exactly what is going on and what can be done to help your condition. Your treamtmet will be tailored to your condition and your rehabilitation program will be commenced.
Follow Up
Depending on your condition a recommended follow up time will be recommended to allow reassessment and progression of your treatment plan and exercises. Many womens health conditions can take time to manage, improve or resolve so patience, consistency and progression of your rehabilitation program is crucial.
What treatment options are available for women’s health conditions?
Treatment of women’s health conditions involve so much more on top of pelvic floor exercises.
Depending on your condition treatment may involve:
- Very specific pelvic floor rehabilitation exercises to suit your current function (strength, endurance, coordination)
- Pelvic floor muscle relaxation exercises
- Manual therapy and hands on treatment (if needed) for release and pain management
- Dry needling and acupuncture for release and pain management
- Abdominal muscle strength and control exercises
- Electrical stimulation for pelvic floor strengthening
- Electrical stimulation for pelvic pain
- Breathing retraining
- Transtibial nerve stimulation for Overactive Bladder
- Dilator therapy
- Bladder retraining drills
- Lifestyle modifications
- Rehabilitation of hip, low back and trunk weakness and imbalances
- Hip mobility and hip releases
Pre & Postnatal Care
Pregnancy & the Pelvic Floor
There are many benefits to getting a pelvic floor assessment during pregnancy rather than waiting until your postnatal assessment. A pelvic floor assessment during pregnancy can help to:
Ensure you perform your pelvic floor contraction correctly:
Research indicates that up to 60% of women with pelvic floor issues (including prolapse or incontinence) incorrectly contract their pelvic floor muscles. Physios love to ensure you are confident with and correctly performing your pelvic floor exercises to keep you strong and leak free.
Help prevent leakage during pregnancy:
Evidence suggests those who do pelvic floor muscle training in pregnancy reduce their risk of urinary incontinence in later pregnancy by 62%.
To help prevent leakage postnatally:
Evidence suggests those who do pelvic floor muscle training in pregnancy reduce their risk of urinary incontinence at 3-6 months postnatal by 29% compared to women who do not do pelvic floor muscle training during pregnancy.
To enhance pelvic floor recovery postnatally:
The more you focus on strengthening your pelvic floor during pregnancy and the better you get at contracting your pelvic floor the easier it will be to commence your pelvic floor rehabilitation program postnatally.
Help address current leakage or prolapse symptoms:
Pelvic floor muscle training can help address and reduce any leakage or prolapse symptoms that you may be experiencing during pregnancy. Symptoms of prolapse may include a heaviness or bulging feeling vaginally, pelvic pain, or difficulty emptying your bladder or bowel.

Prepare the pelvic floor for labour and teach you perineal massage:
Towards the end of pregnancy it is important to focus on relaxation of the pelvic floor to prepare for labor. Perineal massage is a technique used from 35 weeks to help stretch the perineum and the pelvic floor muscles in preparation for birth. Evidence shows that for first time mums perineal massage can help reduce the risk of tears, and reduce the need for episiotomies.
Pregnancy Pain & Treatment
Pregnancy is such an exciting journey to be on, however sometimes there are some changes happening in your body that aren’t so great, such as onset of pain. If you are experiencing pain and discomfort in your pelvis, low back, upper back and ribs we can help you through targeted Physio treatment and exercise.
The most common areas to experience pain during pregnancy include the low back, the upper back, the ribs and the pelvis (known as pelvic girdle pain). Pelvic girdle pain includes pain at the front of the pelvis (the pubic symphysis) and pain at the back of the pelvis (the sacroiliac joints).
Low back and pelvic girdle pain occur in up to 70% of pregnant women. The most common time period for pelvic girdle pain to occur is between 14 and 30 weeks.
Why is pain so common during pregnancy?
Pain during pregnancy is multifactorial however contributing factors include:
- Hormonal changes contributing to ligament laxity and reduced pelvic stability
- Increased load and pressure on the pelvis and low back from growing bub
- Increased lumbar lordosis (or curvature of your low back)
- Changes to spinal biomechanics as bub grows
- Posture changes
Treatment of pregnancy pain will depend on your diagnosis and contributing factors. Treatment may include:
- Releasing of muscles
- Dry needling and acupuncture
- Taping
- Pelvic support belts
- Exercises to help release muscles, stretch muscles, improve mobility, improve strength and reduce pain
- Advice around modifying your activities
- An exercise program to enable you to stay as active and as strong as possible
Despite increasing weight and pressure on the pelvis as the pregnancy progresses, it is still possible to reduce your pain and improve your function during pregnancy.

Labour Preparation
Did you know there are multiple things you can do towards the end of your pregnancy to assist in preparing the pelvic floor for labour and to help reduce your risk of tearing.
Pelvic floor relaxation
During pregnancy it is very important to focus on strengthening the pelvic floor, however towards the end of pregnancy it is also essential to focus on relaxation of the pelvic floor to prepare for labor. Training the coordination between contraction and relaxation will allow you to identify how to relax during the pushing phase of labour.
Perineal massage
Perineal massage is a technique used from 35 weeks to help stretch the perineum and the pelvic floor muscles in preparation for birth. Evidence shows that for first time mums perineal massage can help reduce the risk of tears, and reduce the need for episiotomies. In women who have had a previous vaginal delivery, perineal massage can help to reduce the chance of having ongoing perineal pain at 3 months post delivery.
Postnatal Assessment & Rehabilitation
Postnatally you’ll be busy looking after your new addition to your family, however this is one of the most important times to look after yourself and invest in recovery. Postnatal rehabilitation is essential for addressing any current issues but also preventing issues later on in life. The ultimate aim is to get you back to doing what you want to do.
Although postnatal assessments are recommended at 6 weeks it is never too late to have a postnatal assessment and to start addressing any pelvic floor and abdominal muscle issues.
Postnatal assessments are ideally conducted at 6 weeks postpartum and include:
- A full history of your pregnancy and delivery (whether it be vaginal or c-section)
- A full history of your previous pelvic floor function
- A pelvic floor assessment to determine:
- Pelvic floor muscle strength and endurance
- Pelvic floor tone
- If any pelvic organ prolapse is present
- Your risk of pelvic organ prolapse
- An abdominal muscle separation assessment to determine if separation is present and to what degree
- A pelvic, low back and hip assessment to determine if any pain or weakness/muscle imbalances around the area is present
- Setting your goals you wish to achieve including activities you would love to get back to (whether it be running, lifting weights, pilates or just being active with your kids)
Your postnatal rehabilitation plan will be individualised depending on your assessment and your goals you wish to achieve. Your postnatal program may aim to:
- Improve pelvic floor muscle weakness
- Rehabilitate the pelvic floor following tearing (whether it be a 1st, 2nd, 3rd or 4th degree tear)
- Reduce abdominal separation and restore core strength/control
- Promote recovery after a c-section (including scar management and mobility)
- Address urinary incontinence, or bladder urgency and frequency
- Improve sexual function, including reducing pain with intercourse
- Address bowel incontinence
- Improve pelvic, low back and hip stability and strength
- Address postnatal pain
- Speed up your recovery and help you return exercise


Abdominal Muscle Separation
Abdominal muscle separation is very common postnatally. It occurs when the linea alba (the line of connective tissue down the centre of your rectus abdominus or your “six pack muscle”) becomes stretched, and your rectus abdominus muscle separates as a result.
Physical assessment involves looking at your:
- Posture
- Movement patterns
- Breathing mechanics
- Abdominal muscle strength and function (including rectus abdominis, obliques and transverse abdominis)
- Level of activation of your core
- Degree of separation of the abdominals as well as skin quality
- Doming or coning of the stomach during movements
- Stability of the hips and pelvis
- This will give us the recipe for how we can work together to rebuild your core activation and strength and re-tension through the linea alba.
Your rehabilitation program will involve specific and targeted pelvic floor and core strengthening exercises. There is no “best” exercise or one size fits all approach. Each person requires an individualised program to assist in addressing movement patterns, and optimising core function and activation to rehabilitate the separation. Your program will be progressed as you continue to make improvements in core activation and control. Progression will involve adding in movements to make the exercises functional and relatable to your everyday life.
C-section Recovery
Around 30% of babies in Australia are born by Caesarean delivery, or C-section. During the surgery, the lower portion of your abdominal muscles are cut and hence your body needs time to heal afterward. Physiotherapy can assist in improving recovery from a C-section in the following ways:
- Improving scar tissue mobility
- Desensitising your scar
- Restoring core strength and stability
- Assessing when you are ready to return to certain exercises and activities
- Utilising abdominal compression garments (such as SRC recovery shorts to aid recovery)
Postnatal Back, Neck & Wrist Pain
Low back and pelvic pain
Up to 75% of women who suffer from pregnancy related back pain may continue to have pain postnatally. 40% of women who have back pain postnatally may continue to experience pain beyond 6 months.
Back pain and pelvic girdle pain may persist after birth for many reasons including:
- Hormonal changes
- Reduction in abdominal, hip and low back strength
- Reduced hip and pelvic stability
- Abdominal separation
- Pelvic floor dysfunction
- Repetitive postures
- Incorrect exercise regime or returning to certain exercises before you are ready
A detailed assessment can help determine the reason for your pain and helps develop a comprehensive rehabilitation program to resolve these issues. Manual therapy and dry needling can assist in reducing your symptoms and pain while we get you strong.
Neck and upper back pain
Repetitive movements and postures such as feeding position, looking down at your baby, carrying your baby on the same side and placing them over the same shoulder can place increased strain on the neck and upper back. Often muscle imbalances, including tight muscles and weak muscles may contribute to your pain.
Symptoms may include pain in the neck or upper back, restriction in movement when turning your head, headaches and upper back stiffness. Physiotherapy can be beneficial in reducing pain and preventing it from returning.
Wrist and thumb pain
Up to 50% of women experienced wrist pain in the postnatal period. The most common cause of wrist and thumb pain postnatally is a condition called De Quervain’s Tenosynovitis. In this condition the tendons and/or sheaths around the tendon become thickened and inflamed.

Signs and symptoms include:
- Pain and/or swelling around the base of the thumb, and side of the wrist
- Increased pain with thumb and wrist movements
- Pain associated with lifting, gripping and twisting objects
Treatment may include taping and splinting, modification of movements to reduce load through these structures and a graded strengthening program to reduce pain and restore function.
Postnatal Return to Sport & Running
Knowing when you are able to return to running or high intensity exercise postnatally can be frustrating, particularly with all the conflicting information out there.
Information circling around the internet often promotes 12 weeks as the “magic number” for ladies being able to return to running and high impact exercise postnatally. Unfortunately there is no set time frame that will ensure you are safe to return to running. Instead, a comprehensive assessment ensuring you meet set criteria for pelvic floor function, abdominal rehabilitation and muscle strength is the gold standard for ensuring you are ready.
On top of a standard Postnatal Physio Assessment extra assessments and tests will be performed to determine if you are ready to return to running. This may include:
- A pelvic floor stress test: to determine how well you tolerate impact and jumping activities, if any leakage is present or if any prolapse symptoms are present
- Pelvic floor assessment: to determine your pelvic floor strength and endurance, and if any prolapse is present/your risk of prolapse. Depending on the exercise you are wanting to return to you we will have a set number of contractions and length of holds you should be able to achieve to show that your pelvic floor is ready for the demans of the exercise
- Abdominal assessment: to determine core strength and control, and assess if any abdominal separation is present
- Muscle strength assessment: to determine your leg strength (including the strength of your calf, quadricep, glutes and hamstring muscles). If you return to running without having done any strength training then other injuries are more likely to develop.
What happens next?
If your pelvic floor, abdominals or muscle strength is not quite where it needs to be for return to running we will ensure you are performing a targeted rehab program to address any areas that are lacking.

Birth Related Trauma & Injuries
The most common injuries sustained during childbirth include perineum and pelvic floor tears.
What is a perineal tear?
As the name suggests perineal tears involve tearing of the perineum (area between your vagina and anus). There are four degrees of perineal tears. Up to 85% of females who undergo a vaginal delivery will suffer from some degree of perineal tearing.
How can Physio help with perineal tears?
Pelvic floor Physio is important for everyone postnatally regardless of whether you have a vaginal delivery or c section, however after sustaining a perineal tear it is particularly important for pelvic floor rehabilitation and preventing future issues.
Due to the trauma of a perineal tear the pelvic floor muscles become weakened, may become very sensitive and painful around the scar, and may lead to painful intercourse (dyspareunia).
Pelvic floor physiotherapy can assist in:
- Aiding pelvic floor rehabilitation
- Addressing and preventing urinary and faecal incontinence
- Providing education on scar massage and desensitisation to prevent long term sensitivity and pain in the area
- Addressing pain with intercourse
- Restoring pelvic floor strength and function
Pelvic Health Conditions
Pelvic Organ Prolapse
What is Pelvic Organ Prolapse (POP)?
Pelvic organ prolapse occurs when any of the pelvic organs (bladder/urethra, uterus/cervix, or rectum/bowel) descend downward into the vaginal canal.
How common is prolapse?
Often women feel alone if they are experiencing prolapse as they feel like they are unable to speak up, or feel like no one else is going through the same issue. However prolapse is one of the most common health problems in Australia. Up to 75% of women will develop some degree of prolapse during their life and 1 in 3 women will have prolapse to the level of the vagina.
Symptoms of prolapse often vary depending on the type of prolapse. Symptoms may include:
- A vaginal lump or bulge
- A dragging or heavy sensation vaginally
- Vaginal laxity or looseness
- Dyspareunia (pain with intercourse)
- Low back, pelvic or lower abdominal pain
- Straining to pass urine, or having an intermittent stream (due to urethral compression or kinking)
- Straining to pass a bowel motion, and incomplete bowel emptying
- Recurrent urinary tract infections (due to incomplete emptying resulting in a chronic residual volume)
- Nocturia (due to accumulating residuals during the day)
How can Physio help with prolapse?
Evidence suggests the conservative management of prolapse through physio can be very effective. Physio can help by:
- Providing a thorough assessment to determine what type and grade of prolapse is present, and what your pelvic floor strength and function is like
- Commencing an individualised pelvic floor muscle training program to increase the upward support on the pelvic organs
- Retraining the correct use of abdominal and core muscles
- Optimising bladder and bowel function
- Providing advice on appropriate exercise and activities
- Recommending a pessary (if it is appropriate for your case). A pessary is a silicone device inserted in the vagina to support the pelvic organs, reduce symptoms of prolapse and improve bladder and bowel emptying. For more information on pessaries click here.
Can I get back to exercise with a prolapse?
YES – with the right assessment and treatment plan we can help to improve pelvic floor function and reduce prolapse symptoms. A pessary can be a great option for providing pelvic organ support while allowing safe return to exercise.
Urinary incontinence (Leakage)
Urinary incontinence (or leakage) is the involuntary loss of urine, ranging in severity from just a small leak to a complete loss of bladder control. Incontinence is an extremely common issue affecting up to 1 in 3 women. Incontinence often impacts the ability for women to continue to participate in activities they love, whether it be physical activity or running around with their kids.
The great news is, incontinence can be very well managed, and in most cases, completely resolved with conservative management.
Types of urinary incontinence:
Stress Urinary Incontinence (SUI)
Stress Urinary Incontinence is the involuntary loss of urine associated with activities that increase your intra abdominal pressure and increase pressure down on the pelvic floor. This may include leakage with coughing, sneezing, laughing, running and jumping.
High quality evidence shows that pelvic floor muscle training is very effective in treating stress urinary incontinence. It is essential that the pelvic floor muscle exercises are performed correctly, including the right prescription of intensity and type of pelvic floor exercises to treat your issue.
Urge Urinary Incontinence (UUI)
Urge Urinary Incontinence (UUI) is the involuntary loss of urine associated with the urge to pass urine. It is often associated with a strong or sudden urge to pass urine that you are unable to hold (Overactive Bladder). Treating UUI is more complex than SUI, and may involve a range of different treatment options including pelvic floor muscle training, pelvic floor down training, TENS for bladder downtraining, urge suppression techniques, bladder retraining drills and education around bladder irritants.
A Women’s Health assessment will help identify what type of incontinence you have, and provide an individualised and evidence based treatment plan to help you address your incontinence and achieve your goals.
Overactive Bladder (OAB)
Overactive Bladder (OAB) causes a frequent and sudden urge to urinate that may be difficult to control.
Symptoms of OAB include:
- Urgency: feeling a sudden urge to urinate that’s difficult to control
- Frequency: going to the bathroom to pass urine > 8 times in 24 hours
- Nocturia: Waking up at night to pass urine more than once
- Urinary Incontinence: You may or may not experience urge incontinence (urine leakage when you feel the sudden urge to go)
How can Physio help with OAB?
Conservative management is recommended as the first-line treatment for OAB. Through a comprehensive assessment we will be able to determine contributing factors for your OAB and determine an individualised and specific treatment plan to best overcome the issues. Treatment options may include:
- Treatment of modifiable risk factors
- Reduction of exposure to bladder stimulants
- Improving bladder and bowel habits
- Fluid optimisation
- Pelvic floor muscle training
- Treating pelvic floor dysfunction
- Bladder and behavioural retraining drills and programs
- Urge suppression strategies
- Transtibial nerve stimulation for bladder down training

Endometriosis Pain
What is Endometriosis?
Endometriosis is a condition in which cells similar to those that line the uterus are found in other parts of the body. These endometrial cells can deposit anywhere in the body however are most commonly found in the pelvic area.
Common symptoms of endometriosis include:
- Painful periods (pain that last > 1-2 days that does not settle with over the counter pain relief)
- Painful ovulation
- Pain during or after sexual intercourse
- Heavy bleeding (with or without clots)
- Chronic pelvic pain
- Severe pain that means you can’t participate in work, school or sporting activities.
- Fatigue
- Infertility
- Pain with bowel movements or urination.
- Bladder urgency/frequency
- Bleeding from the bladder or bowel.
- Change in the pattern of bowel habits, such as constipation, diarrhoea.
- Increased abdominal bloating (With or without pain at the time of the period)
How can the pelvic floor and other pelvic/abdominal musculature contribute to pain?
Common musculoskeletal changes with endometriosis includes:
- Spasm of the pelvic floor muscles in response to pain
- Apical breathing with a braced abdominal wall
- Myofascial trigger points in the pelvic floor, abdominal muscles, hip and low back muscles
- Pelvic floor muscle hypertonicity or overactive (which can contribute to bladder and bowel dysfunction including increased urinary frequency/urgency and difficulty emptying the bladder or bowel)
Understanding and improving pelvic floor muscle function is essential for good bladder, bowel and sexual function. Addressing pelvic floor function can help to improve your bladder, bowel and sexual function because they are all connected and related.

How can Physiotherapy help manage my endometriosis pain?
Physiotherapy aims to help you better understand your condition and how you can manage your pain and symptoms. There are many things that we can work on together to reduce your pain and symptoms. some important things we may focus on include:
- Pain management
- Pelvic floor down training
- Dilator therapy
- Desensitisation of the nervous system
- Pelvic stretching and releasing
- Restoring proper muscle function:
- TENS for pain modulation
- Exercise
Overactive Pelvic Floor Muscles
Pelvic floor muscle overactivity is a condition where there may be increased pelvic floor muscle tension at rest, or a decreased ability to fully relax the pelvic floor muscles. People often recognise that pelvic floor underactivity or weakness is a common issue, but may not realise that an overactive pelvic floor can cause just as many issues.
Signs and symptoms of an overactive pelvic floor:
- Not being able to feel a pelvic floor muscle contraction or release
- Pelvic pain (may include urethral, vaginal, rectal, lower abdominal pain)
- Coccyx (tailbone) pain
- Low back pain
- Urinary urgency or frequency (getting a strong urge to go to the toilet or needing to go frequently)
- Slow urinary flow or the feeling of incomplete bladder emptying
- Pain with sex, either with initial or deep penetration
- Difficulty or pain inserting tampons
- Difficulty or pain with emptying the bowels or passing ‘skinny stools’
- Stress urinary leakage in some cases (leakage with cough/sneezing/run/jump)
As you can see from the above symptoms an overactive pelvic floor may present very similar to a weak or underactive floor. This is why an assessment to determine if your pelvic floor is over or underactive is essential. Overtraining or constantly focusing on tightening and strengthening an overactive pelvic floor will lead to a worsening of your symptoms rather than an improvement
An assessment to determine why your pelvic floor is overactive, and if it is overactive and strong or overactive and weak is essential to determine a specific pelvic floor training program will be best suited to you.

Underactive (Weak) Pelvic Floor Muscles
Weakness of the pelvic floor muscles is an extremely common issue. Symptoms of an underactive pelvic floor may include:
- Urinary incontinence/leakage (with coughing/sneezing/running/jump or when you have a strong urge to pass urine)
- Urgency and frequency of needing to pass urine
- Inability to control ‘wind.’
- Low back and pelvic pain
- In ability to use tampons
- Pelvic organ prolapse symptoms, such as heaviness or bulging sensation vaginally
What can contribute to an underactive pelvic floor?
- Pregnancy and childbirth (particularly involving prolonged labour or the use of forceps)
- History of chronic respiratory conditions and chronic cough
- History of chronic constipation or straining
- Regular heavy lifting
- Elite and high level athletes involving high impact and high loads. For example gymnastics, running and weight lifting
- Obesity
- Age: pelvic floor muscle mass reduces as we age
- Hormonal changes ie reduce oestrogen with menopause
- Pelvic and abdominal surgeries

A pelvic floor assessment will help determine if your pelvic floor is overactive or underactive. Depending on the ability of your pelvic floor muscles to activate there are different treatment options available to help strengthen your pelvic floor. This may include a specific and individualised pelvic floor muscle training program, electrical stimulation for the pelvic floor, and pelvic floor muscle training devices.
Pelvic Pain (including pain with intercourse)
Pelvic pain is a significant problem that affects up to 25% of the population, and can have a massive impact on quality of life. Many women live with chronic pelvic pain (pain lasting over 3 months) and often struggle to find a diagnosis. Pelvic floor Physio can assist in assessing, diagnosing and treating many pelvic pain conditions.
Symptoms of pelvic pain conditions:
Symptoms vary person to person, and depend on the condition and the severity however some common symptoms include:
- Pelvic, hip, abdominal or back pain
- Dull aching
- Sharp pains or cramping
- Pressure or heaviness deep within the pelvis
- Pain with or inability to use tampons
- Dyspareunia (pain with intercouse)
- Pain after intercourse
- Pain while having a bowel movement or urinating
- Pain when you sit for long periods of time
Vaginismus
Vaginismus is the involuntarily contracting and tightening of the pelvic floor muscles. It can happen before/during intercourse, when inserting a tampon, or during a gynaecological examination. Vaginismus can cause pain and discomfort and may prevent sexual penetration. It can also make it impossible to undergo a pelvic examination.
Vulvodynia
Vulvodynia is ongoing pain (usually described as a burning pain) in the vulva (the female genital area). The exact cause is unknown but it appears that the nerve endings in the skin of the vulva become over sensitive and send abnormal signals which are felt as a sensation of pain. Vulvodynia affects up to 15% of the population.
How can Physio help with pelvic pain?
A women’s health assessment can help to determine the cause of your pain and factors that need to be addressed. As chronic pelvic pain can be complex and multifactorial we will work together to find a treatment plan best suited to you.
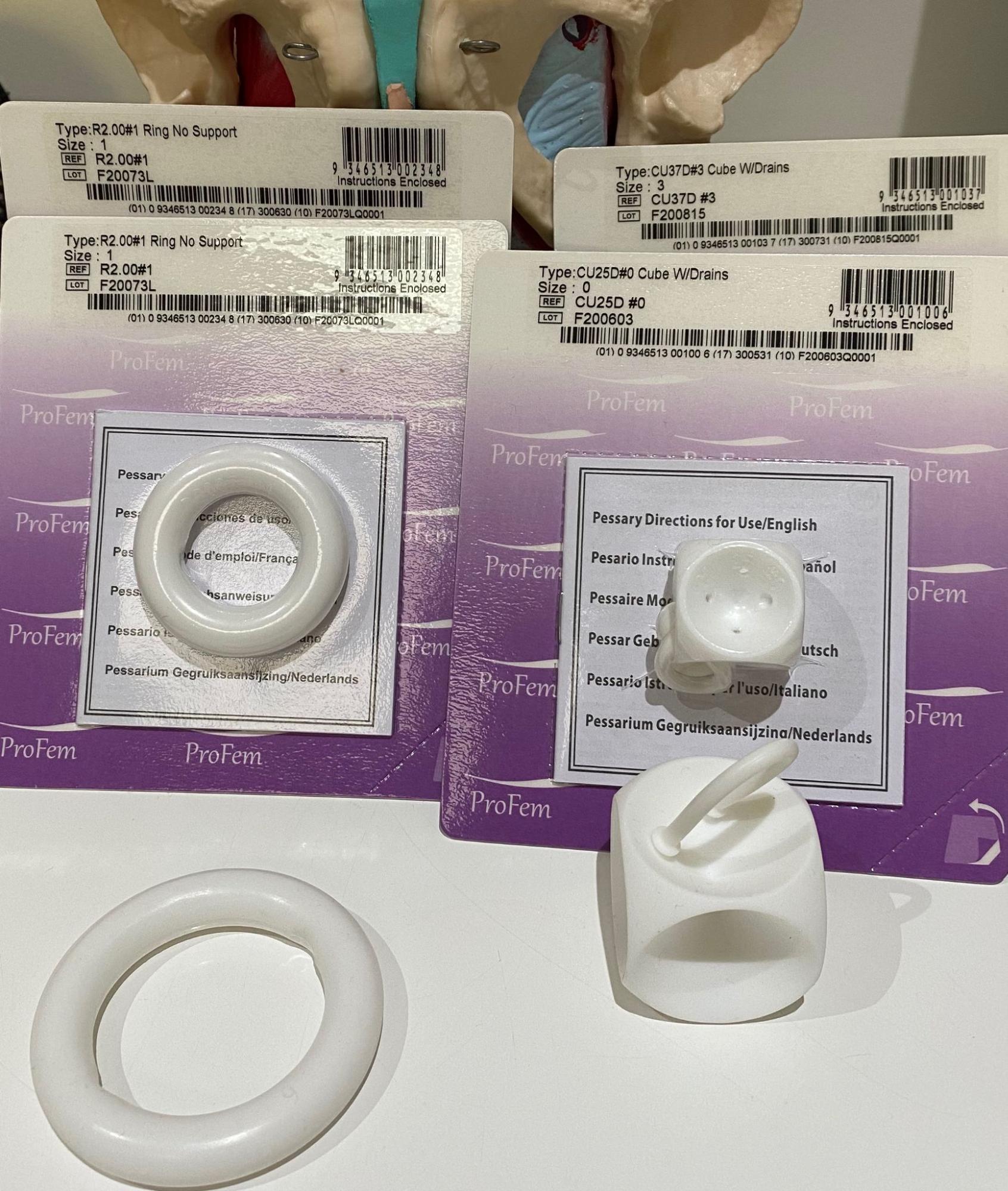
Pessary Fittings
What is a Vaginal Pessary?
A pessary is a silicone device that is inserted into the vagina to help support a prolapse of the pelvic organs (including the uterus/cervix, bladder/urethra and bowel/rectum). Pessaries can also be used to help reduce stress urinary incontinence (leakage with coughing/sneezing/running/jumping)
A pessary is a great non-surgical way to treat and manage pelvic organ prolapse and incontinence. Vaginal pessaries have been proven to be as successful as surgery in relieving prolapse symptoms.
How does a pessary work?
The pessary sits high inside the vagina. When it is in the correct position you should not be able to feel it. After the pessary has been inserted you can resume all of your normal day to day activity. In fact the pessary should improve your ability to be active as it supports the prolapse and should make you feel more comfortable.
If you feel the pessary is not working well, it can easily be removed.
What are the benefits of using a pessary?
The benefits of using a pessary are that it:
- Can reduce or lessen the symptoms of vaginal prolapse
- Does not stop you from being able to have sex
- Is less invasive (and as a result, less complicated) than surgery.
- Can allow you to return to exercise without worsening your prolapse
- May allow some recovery of your prolapse
- May reduce incontinence
How is the pessary inserted?
- The pessary is easy to insert. It is inserted into the vagina (similar to a tampon)
- Your Physiotherapist will do an assessment to determine the right size and style of pessary best suited to you. Sometimes a number of sizes need to be tried to find the right size for you.
- Your Physiotherapist may teach you how to remove, clean, and reinsert the pessary on a regular schedule. If it’s hard for you to remove and replace your pessary, you can have it done regularly with your Physiotherapist.
Are there any risks?
- As long as your pessary is correctly fitted and you follow the correct hygiene procedures there is minimal risk of pressure areas or infection
- It is important that you see your Physiotherapist every six to twelve months to have the pessary changed and to check the vagina. You should also have an annual check with your GP to check for any signs of infection.
- There is no risk of the pessary being lost inside the vagina
How often does the pessary need to be replaced?
- Your pessary will need to be replaced every 12 months